Infectious Disease and Inflammation Models
Infectious Disease
Living tissues are protected against microbial infection by an array of physical, chemical, and immunological barriers that vary between body sites, organ systems, and host species. Scientists at Queen Mary University of London (QMUL) study how bacteria, viruses, and fungi interact with these barriers to cause disease, including disorders of microbial dysbiosis (e.g. inflammatory bowel disease [IBD]), and a diverse range of acute / chronic infections. Among these activities, theme lead Dr McCarthy is developing a novel ‘gut-on-chip’ model of fungal invasion via the intestine (implicated in IBD and a major cause of lethal sepsis in cancer); Prof Pennington is developing an alveolus model of the immune response to respiratory viruses (including SARS-CoV-2); Dr Chambers is using organ chip technology to study how lung tissue aging modifies infection risk; Prof Alazawi and Dr Dufton are using organoid approaches to explore mechanisms of chronic liver inflammation; Dr Wareham is assessing anti-microbial resistance in nosocomial pathogens; Dr Bourke is using epithelial integrity assays to study diet-bacterial interactions with host tissue physiology.
By studying host-microbial interactions across a wide range of bacterial, viral, and fungal species, QMUL researchers aim to reduce the future burden of known and emerging infectious diseases (as well as the acute/chronic inflammatory disorders that frequently stem from these).
Inflammation
Inflammation is a major research area at QMUL, bringing together expertise in bioengineering, nanomedicine, and organ-on-chip technology to understand key mechanisms of acute and chronic human disease. Many of these basic and applied research activities are coordinated through the interdisciplinary, cross-institute Centre for inflammation and Therapeutic Innovation (CiTI).
QMUL is renowned for its pioneering research into inflammatory processes, with international leadership on the mechanisms that regulate cell trafficking (Dr Cooper, Prof Marelli-Berg), vascular pathology (Dr Nightingale, Dr Whiteford, Dr Dufton), adaptive immunity (Dr Longhi), inflammaging / immunosenesence (Dr Henson, Dr Lewis, Dr Chambers, Dr Montero-Melendez) and the mechanisms that drive active resolution of inflammation (Prof Perretti, Dr Norling, Prof Dalli). These programmes integrate with QMUL’s research activity in host-microbe interactions (summarised above), where infection risk often depends on host inflammatory status, vascular dissemination of invading pathogens, and the anti-microbial immune responses that ensue.
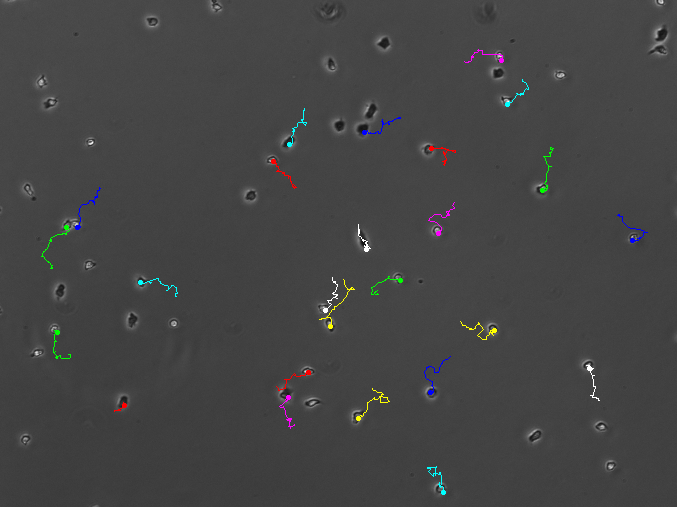
The QM+Emulate Organs-on-Chips Centre is key to advancing these complementary programmes, allowing the human biology of different organs to be replicated accurately in vitro. By incorporating relevant cell types and tissues cultured under appropriate levels of fluid flow and mechanical stretch, our researchers can determine how relevant stimuli (e.g. breathing / peristalsis) shape the dynamics of infection, immunity, and inflammation in human tissues in vivo.
People
- Dr Vahitha Abdul Salam
Lecturer, Queen Mary University of London - Dr Ezra Aksoy
Lecturer, Queen Mary University of London - Dr Kieran Bates
Lecturer in Microbiome Science, Queen Mary University of London - Dr Claire Bourke
Lecturer/Research Fellow, Queen Mary University of London - Dr Ana Caetano
Clinical Senior Lecturer, Queen Mary University of London - Dr Sean Carlson
NHS Clinician / Researcher, Queen Mary University of London - Dr Emma Chambers
Lecturer, Queen Mary University of London - Dr Tina Chowdhury
Reader in Regenerative Medicine, Queen Mary University of London - Prof John Connelly
Professor of Bioengineering, Queen Mary University of London - Prof Jesmond Dalli
Professor in Molecular Pharmacology, Barts and The London School of Medicine and Dentistry - Dr Neil Dufton
Lecturer in Inflammatory Sciences, Queen Mary University of London - Dr Marc Fernandez-Yague
Lecturer in Chemistry, Queen Mary University of London - Prof Martin Knight
Professor of Mechanobiology, Dean for Research, Queen Mary University of London - Dr Yung-Yao Lin
Senior Lecturer, Queen Mary University of London - Prof Adrian Martineau
Professor of Respiratory Infection & Immunity, Queen Mary University of London - Dr Simon McArthur
Reader in Systems Neurobiology, Queen Mary University of London - Dr Neil McCarthy
MRC Career Development Fellow; Senior Lecturer in Immunology, Queen Mary University of London - Dr Vito Mennella
Associate Professor, Reader in Nanoscale Biology, Queen Mary University of London - Dr Tom Nightingale
Senior Lecturer, Queen Mary University of London - Dr Lucy Norling
Versus Arthritis Senior Fellow, Queen Mary University of London - Prof Sussan Nourshargh
Head, Centre for Microvascular Research, Queen Mary University of London - Prof Venet Osmani
Professor of Clinical AI and Machine Learning, Queen Mary University of London - Prof Daniel Pennington
Professor of Molecular Biology and Centre Lead for Immunobiology, Queen Mary University of London - Prof Mauro Perretti
Professor of Immunopharmacology, Queen Mary University of London - Prof Greg Slabaugh
Director of the Digital Environment Research Institute, Queen Mary University of London - Dr Egle Solito
Reader in Immunobiology, Queen Mary University of London - Dr Claire Villette
Lecturer in Computational Bioengineering, Queen Mary University of London


